Oral Health, An important part of general health
Introduction
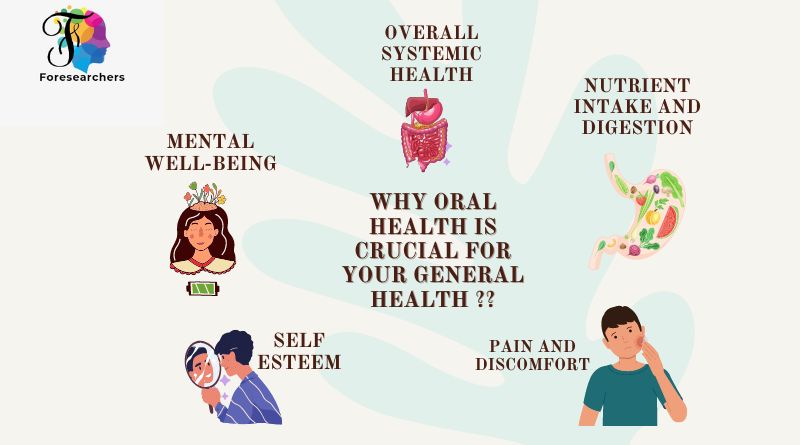
Yes, oral health is indeed an important part of general health. The health of your mouth, teeth, and gums can have a significant impact on your overall well-being. Here are a few reasons why oral health is crucial for your general health:
- Overall Systemic Health: Poor oral health has been linked to various systemic health conditions, including cardiovascular disease, diabetes, respiratory infections, and pregnancy complications. Maintaining good oral hygiene can help reduce the risk of these conditions.
- Oral-Systemic Connection: There is a strong connection between oral health and the rest of the body. For example, gum disease (periodontitis) has been associated with an increased risk of heart disease and stroke. Bacteria from the mouth can enter the bloodstream and contribute to inflammation and other health problems.
- Nutrient Intake and Digestion: Your oral health can impact your ability to chew and digest food properly. Healthy teeth and gums are essential for efficient chewing, which promotes proper digestion and nutrient absorption.
- Pain and Discomfort: Dental problems such as tooth decay and gum disease can cause pain, discomfort, and difficulty eating, which can lead to poor nutrition and overall health issues.
- Self-Esteem and Mental Well-being: Oral health also plays a role in your self-esteem and mental well-being. Problems like missing teeth, bad breath, or visible dental issues can affect your confidence and social interactions, leading to emotional distress and a lower quality of life.
To maintain good oral health, it’s important to practice regular oral hygiene habits such as brushing your teeth at least twice a day, flossing daily, and visiting your dentist for routine check-ups and cleanings. Additionally, adopting a healthy diet, limiting sugary foods and drinks, and avoiding tobacco use can contribute to better oral and general health.
To maintain good oral health, it’s important to practice regular oral hygiene habits such as brushing your teeth at least twice a day, flossing daily, and visiting your dentist for routine check-ups and cleanings. Additionally, adopting a healthy diet, limiting sugary foods and drinks, and avoiding tobacco use can contribute to better oral and general health.
Oral health is closely related to systemic health. Periodontitis, a chronic inflammatory disease which is highly prevalent worldwide, interacts with a variety of noncommunicable diseases (NCDs). It is a risk factor in the complex pathogenesis of diabetes mellitus and cardiovascular disease and plays a role in the development of endocarditis and recurrent pneumonia in elderly people. However, the available data may be interpreted in different ways, and more and better-designed studies are still needed to answer relevant questions about the causal role of periodontitis in NCDs.
Bacterimia and Endocarditis
Historically, the relationship of periodontitis with systemic health is illustrated by its role as a risk factor for endocarditis. Bacteremia, defined as the entry of bacteria into the blood stream8, is one precondition for endocarditis. It can be initiated by any mechanical action on the skin or the mucosae. The amount and the frequency of bacteremia originating from the oral cavity depend on both the invasiveness of the mechanical action and the degree of inflammation at the interface between the hard and soft tissues. The vast majority of bacteremia do not cause endocarditis, even in patients at high risk. However, in high-risk patients, the more frequently and the more intensely bacteremia occurs, the likelihood of endocarditis will increase.
Periodontal therapy can have a protective effect in people at risk of endocarditis, and its importance has led to new guidelines for the dental treatment of such patients. The guideline only recommends the preventive use of antibiotics in patients with the highest risk of endocarditis. It advises against antibiotic prophylaxis in those with medium and low risk due to the hazards of such medication13, and the fact that the preventive fraction of antibiotic prophylaxis, even if taken correctly, is only around 50%. The maintenance of a healthy periodontium should therefore be recommended in patients with any increased risk of endocarditis, although the highest degree of evidence is currently with studies using bacteremia as a surrogate marker for the risk of endocarditis.
Diabetes Mellitus
The relationship between diabetes mellitus and periodontitis has been well known for decades, and periodontitis is regarded as one of the complications of poorly controlled diabetes mellitus. In addition, it has also been known that acute inflammation may lead to poor glycemic control. This is due to the fact that infections reduce the uptake of glucose into cells, and endotoxins and inflammatory mediators reduce the efficiency of insulin. Due to these pathogenic pathways, periodontitis has long been regarded as a risk factor for poor blood glucose control in diabetes patients. To test this hypothesis, numerous randomized controlled clinical trials have been performed, all addressing the change in HbA1c after periodontal treatment. Several systematic reviews have condensed these results. Although there is some heterogeneity, the systematic reviews come to the conclusion that mechanical periodontal therapy ‘associates with approximately a 0.4% reduction in HbA1c at 3 months, a clinical impact equivalent to adding a second drug to a pharmacological regime for diabetes’.
However, it is important to remember that the effect of periodontal therapy on the individual patient’s HbA1c levels is not predictable. It may be that only a small fraction of patients contributed to the average reduction of blood glucose values and that for the majority, HbA1c values remained unchanged or even increased after periodontal therapy. The result of such therapy with respect to HbA1c levels may significantly differ from patient to patient. However, a broad awareness of this relationship should be familiar to both professionals and patients. Based on the scientific evidence, the European Federation for Periodontology (EFP)/American Academy of Periodontology (AAP) recommend that patients with diabetes should be monitored carefully and periodontitis, if present, should be treated promptly.
As early as 1963, Mackenzie and De Millard observed that patients with atherosclerosis had 62% more alveolar bone loss compared to healthy controls. This association was also seen in large cohort studies, although some of them have been criticized for not correcting for confounding variables such as smoking, which would prevent the associations from becoming statistically significant. However, a potential pathologic pathway exists as the inflammatory burden contributes to atherosclerosis, and periodontal pathogens are found in atherosclerotic vessel walls. Moreover, it has been shown in animal models that periodontal pathogens initiate the formation of atherosclerotic plaques and Porphyromonas gingivalis in particular accelerates the development of atheroma in arterial walls in mice. The ‘proof of principle’ therefore exists, and Beck et al. have published a pathogenic model which hypothesises that there are patients who are susceptible to the side effects of chronic inflammation, and others who are not. To date, we know that there is a broad base of common genetic variants which increase both the risk of cardiovascular disease and the risk of periodontitis adding to other common risk factors for both diseases such as increased blood glucose levels, psychosocial stress and smoking.
Cardiovascular Disease
With this complexity, the potential interaction between cardiovascular disease and periodontitis is therefore both more theoretical and more difficult to prove than that between diabetes mellitus and periodontitis. Moreover, due to financial and ethical issues, no randomised controlled clinical trials on hard endpoints have been performed. Instead, several surrogate parameters have been explored in intervention trials to show the causal role of periodontitis on atherosclerosis. In these studies, it has been shown that periodontitis is associated with endothelial dysfunction of the brachial artery which was reversed by periodontal therapy. Most studies have been performed with C-reactive protein (CRP) as a surrogate parameter, showing a statistically significant reduction due to periodontal therapy. Several systematic reviews have, therefore, pointed out that periodontal therapy reduces surrogate parameters for cardiovascular disease.
However, in a consensus report based on the available evidence, the EFP/AAP conclude that ‘while in vitro, animal and clinical studies do support the interaction and biological mechanism, intervention trials to date are not adequate to draw further conclusions. Similarly to diabetes mellitus, the report shows the heterogeneity of systemic inflammatory responses to periodontal therapy with respect to CRP values and points out that despite the overall reduction of CRP values on the patient level, scaling and root planning resulted in largely inconsistent and unsustainable results, without explanation for such heterogeneity. This may again indicate the role of periodontitis as a risk factor, whose clinical relevance is dependent on a complex interplay of various factors ranging from genetics to behaviour.
Conclusion
Periodontitis is a preventable and treatable disease. Its treatment and prevention are therefore an important goal in itself. However, due to its nature as a chronic inflammatory disease and, as a consequence, the long-lasting inflammatory burden on the whole body, an increasing focus on periodontitis’ causal role in other NCDs has been seen in the last 25 years. In most cases, associations between periodontitis and NCDs have been shown and pathogenic pathways are plausible, but final proof of a causal role has not yet been demonstrated. This is due to the fact that periodontitis and the NCDs are associated with a broad variety of common risk factors, which range from genetic predisposition to health awareness and preventive behaviour. Some data indicate that, on a patient level, different combinations of risk factors may determine the role that periodontitis and periodontal treatment play in other NCDs, but to date, the exact effect cannot be determined. However, periodontitis seems to qualify as one risk factor in the complex pathogenesis of diabetes mellitus, cardiovascular disease, kidney disease and recurrent pneumonia in elderly patients. For other diseases, appropriate clinical studies to prove causality are either lacking or have not shown a clear effect.
Therefore, given the lack of data, the benefit of successful periodontal therapy in terms of effectiveness or efficiency, as well as the contribution of oral conditions to the prevention and control of NCDs, remains unclear. Regardless, it is clear that periodontitis contributes to a chronic inflammatory burden, which is of concern. Independent of the extent to which other NCDs are triggered, modified or caused by periodontitis, communication between physicians and dentists is desirable. Ageing is associated with an increase in risk factors for NCDs. Periodontitis is one of these potential risk factors and is modifiable. This opportunity should be seized.
Therefore, the following three suggestions are offered:
- Collaboration between dentists and physicians is required, and obstacles to the communication and exchange of information should be eliminated.
2. Early detection of NCDs and oral diseases is essential. Interaction between dentists and physicians is necessary to optimize screening.
3. Common risk factors require common/coordinated preventive strategies between dentists and physicians. In particular in tertiary prevention, health promotion measures should be coordinated among oral healthcare providers.
References:
- Abnet CC, Qiao Y-L, Dawsey SM, et al.
Tooth loss is associated with increased risk of total death and death from upper gastrointestinal cancer, heart disease, and stroke in a Chinese population-based cohort
2.Holmlund A, Holm G, Lind L.
Number of teeth as a predictor of cardiovascular mortality in a cohort of 7,674 subjects followed for 12 years
J Periodontol1 (2010), pp. 870-876
3. Mack F, Schwahn C, Feine JS, et al.
The impact of tooth loss on general health related to quality of life among elderly Pomeranians: results from the study of health in Pomerania (SHIP-0)
Int J Prosthodont, 18 (2005), pp. 414-419
4. Marik PE.
Aspiration pneumonitis and aspiration pneumonia
N Engl J Med, 344 (2001), pp. 665-671
5. Ren Q, Yan X, Zhou Y, et al.
Periodontal therapy as adjunctive treatment for gastric Helicobacter pylori infection
Cochrane Database of Systematic Reviews (2016), p. CD009477
6.Scannapieco FA, Cantos A.
Oral inflammation and infection, and chronic medical diseases: implications for the elderly
Periodontol 2000, 72 (2016), pp. 153-175
7. Schwahn C, Volzke H, Robinson DM, et al.
Periodontal disease, but not edentulism, is independently associated with increased plasma fibrinogen levels
Thromb Haemost, 92 (2004), pp. 244-252
Get connected to our social media platforms for more insights on dental health: